The goal/learning objective of marijuana and psychotropics is to understand the interactions between marijuana and a patient’s current psychotropic medications in a clinical experience to gain insight into the potential effects and risks of combining these substances. The objective is to understand how marijuana may interact with a patient’s specific psychotropic medications, including any potential synergistic or adverse effects. By exploring this interaction, healthcare professionals can make more informed decisions and provide personalized advice to patients regarding the use of marijuana alongside their psychotropic medications.
The Goal Objective of Marijuana and Psychotropics and its Application:
This new information about marijuana and psychotropics, combined with prior knowledge and beliefs, carries forward into future practice by enhancing the clinician’s ability to provide comprehensive, individualized care. Understanding the interactions between marijuana and psychotropic medications allows healthcare professionals to have more meaningful discussions with patients about potential risks, benefits, and alternative options. It helps clinicians tailor their treatment plans, considering the patient’s medical history, current medications, and desire to use marijuana for therapeutic or recreational purposes. This knowledge also enables healthcare professionals to provide appropriate guidance, monitoring, and support to ensure the patient’s safety and well-being while using marijuana and psychotropic medications.
Evidence-based about Marijuana and Psychotropics:
Extensive laboratory, clinical, and epidemiological evidence connects marijuana use to cognitive impairment, and clinical and epidemiological data link it to psychosis. The correlations with addiction, anxiety, and depression, however, are based mainly on interviews of national population samples, which are likely to differ from patients who present for treatment. The evidence that marijuana benefits PTSD comes mainly from animal data.
Non-intoxicated regular cannabis users perform worse on global neuropsychological tests by a third of a standard deviation or less. Some evidence suggests this cognitive impairment may be short-term, with recovery occurring over days to months after cessation of use. Its extent and persistence are worse with early age of onset, high frequency, and long duration of use.2 Marijuana-induced cognitive dysfunction may account for its association with motor vehicle accidents at a level that is approaching that of alcohol and reduced life achievement.1 Discussing patients’ marijuana use in high-risk situations, including driving and sexual activity, may be lifesaving, and exploring its effects on academic and work performance may improve outcomes.
Marijuana and Psychotropics related problems
Marijuana-related problems fall well within the reach of psychiatric practice: many patients use marijuana, which is likely to affect their psychiatric symptoms and response to treatment.
For decades, marijuana has been associated with the emergence of schizophrenia and other psychotic disorders. Recent data show that in genetically vulnerable individuals, psychotic disorders are more likely to emerge earlier if marijuana is used.2 Ongoing marijuana use by patients with schizophrenia is associated with worse outcomes.5 Thus, patients with individual or family histories of psychosis can be counseled that marijuana use puts them at greater risk for developing or exacerbating a psychotic illness.
The widely quoted statistic about marijuana’s addictive propensity-that a cannabis use disorder will develop in 9% of people who try marijuana-comes from a national epidemiological sample of 34,653 individuals interviewed from 2001 to 2002 and again from 2004 to 2005. The researchers found marijuana less addictive than nicotine (the corresponding figure is 68%), alcohol (23%), and cocaine (21%). For psychiatric patients, however, the picture is far bleaker.
In the study, individuals with psychotic or conduct disorders who used marijuana had double the risk of addiction; triple the risk of mood, anxiety, and attention deficit disorders; quadruple the risk of personality disorders and alcohol dependence; and cocaine dependence increased the risk by a factor of 6.4 In clinical practice, patients with cannabis use disorder may have great difficulty limiting or abstaining from marijuana use, which exacerbates psychiatric problems, and treatment may need to target marijuana use as well as other issues.
Earlier data associated marijuana with anxiety disorders, and it is precisely that marijuana intoxication elicits panic-like symptoms and even paranoid thinking in some individuals. Recent analyses of population-based data have disagreed about how much excess risk for anxiety disorders can be attributed to marijuana use and how the risk varies among subgroups.9
Marijuana use is every day among patients with PTSD. Animal studies have found that cannabinoids can prevent stress-induced emotional and memory effects, and preliminary studies have found a reduction in some PTSD symptoms in humans. There have, however, been no large-scale, controlled studies.10 Clinicians who treat marijuana-using patients with anxiety or trauma-related disorders will need to explore the relationship of their symptoms to marijuana use on a case-by-case basis.
Although a 2003 review found elevated rates of depression in marijuana users and evidence of depression increasing with ongoing use,11 in more recent analyses, the correlation has dropped out when potentially confounding factors are controlled. 12 Another review found antidepressant medication ineffective in depressed patients with cannabis use disorder.
However, the cited trials had very high placebo response rates, probably because of the intensive psychosocial treatments they provided.13 As with anxiety disorders, it is important to explore with patients the relationship between their marijuana use and depression. Severely depressed patients may have difficulty participating in such explorations, and a trial of abstinence may be the best strategy, which may require psychotherapy or family intervention to implement.
Evidence-based treatments for cannabis use disorder include cognitive-behavioral therapy for addiction, and contingency management, which are modestly effective.14 Pharmacological options are pretty limited: Dronabinol (THC) is effective for cannabis withdrawal, but using it would require a legal waiver. There is limited evidence that gabapentin may relieve cannabis withdrawal symptoms and that gabapentin and N-acetyl cysteine may be helpful for cannabis use disorder.13.
Applying Cultural Knowledge to Marijuana and Psychotropics:
When considering the cultural aspect of a patient, it is essential to recognize that different cultures hold varying beliefs and attitudes toward marijuana and psychotropic medications. For instance, in some cultures, marijuana may have a long-standing history of medicinal or spiritual use, while in others, it may be stigmatized or even illegal.
To address this cultural consideration, healthcare providers should adopt a patient-centered approach. This involves actively listening to the patient’s beliefs, values, and preferences regarding marijuana and psychotropic medications. Engaging in open and non-judgmental discussions can help foster trust and enable the development of a treatment plan that aligns with the patient’s cultural background. Additionally, healthcare providers can offer educational resources tailored to the patient’s cultural context, allowing them to make informed decisions about their healthcare.
Educating Family Members on Marijuana and Psychotropics:
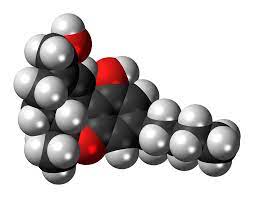
When educating a patient or family member about the interactions between marijuana and psychotropic medications, it is essential to provide accurate and balanced information. Firstly, I would explain that marijuana contains cannabinoids, including THC and CBD, which can interact with psychotropic medications. THC can enhance the effects of certain medications, potentially leading to increased sedation or side effects. Conversely, CBD can inhibit the metabolism of certain medications, causing them to assemble in the body and potentially increase their side effects.
It is crucial to highlight the significance of discussing marijuana use with the prescribing healthcare provider, as they can assess individual risks and benefits, consider potential drug interactions, and make appropriate adjustments to the medication regimen if needed. Open communication with healthcare professionals is critical to ensuring safe and effective treatment.
Challenges Faced In Marijuana and Psychotropics
During this marijuana and psychotropics unit’s clinical experience, I faced a significant challenge in integrating information about the interactions between marijuana and a patient’s current psychotropic medications into their care was the limited research and evidence available on this specific topic. The field of marijuana research is relatively new, and while there is a developing body of literature, it is still evolving. This lack of comprehensive data made it challenging to provide accurate and evidence-based recommendations to the patient. Additionally, individual variations in metabolism, drug sensitivity, and drug-drug interactions further complicate the situation. It required careful consideration, consultation with colleagues, and close patient monitoring to ensure their safety and optimize treatment outcomes.
References:
- American Psychiatric Association: “Diagnostic and Statistical Manual of Mental Disorders” (DSM-5) – The authoritative guide used by mental health professionals to diagnose mental disorders, including those related to psychotropic substances.
- World Health Organization (WHO): “Management of Substance Abuse” – A collection of resources, guidelines, and reports on managing substance abuse, including psychotropic substances. Available at: https://www.who.int/substance_abuse/en/
- National Institute on Drug Abuse (NIDA): “Drugs of Abuse” – A comprehensive resource providing information on various drugs of abuse, including their effects, risks, and treatment options. Available at: https://www.drugabuse.gov/drug-topics





